Congress Passes Surprise Medical Billing Legislation. They define a surprise bill as any bill that gives them a surprise whether its the amount on the bill or services that they werent expecting.
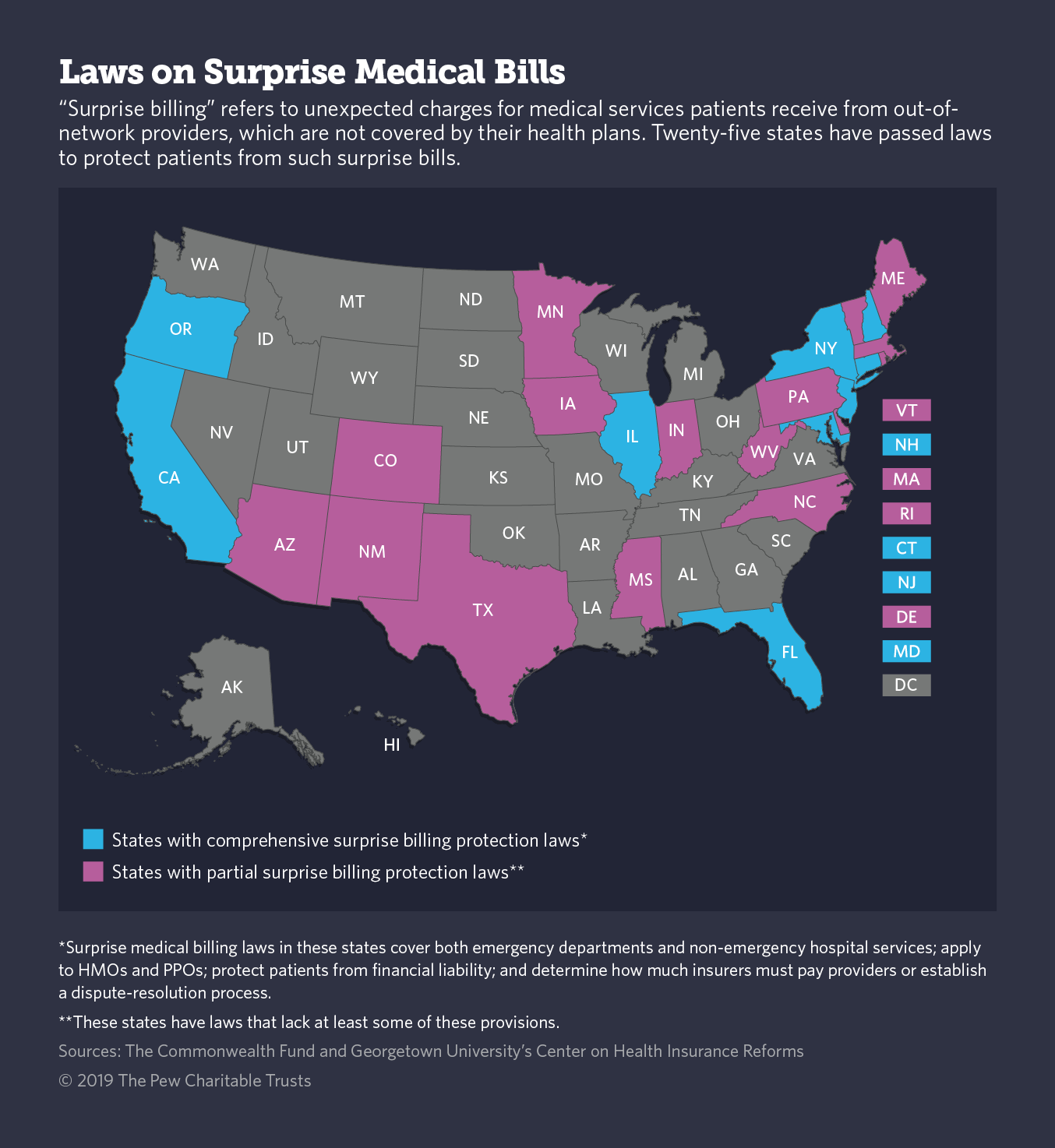
 Balance Billing By Providers Assessing State Consumer Protections
Balance Billing By Providers Assessing State Consumer Protections
In the final days of its 116th meeting Congress passed legislation containing COVID-19 relief and fiscal year 2021 government funding.
Surprise billing law. Federal surprise billing legislation becomes law Differing committee perspectives. The fix will help many consumers. What consumers need to know about surprise or balance billing Starting Jan.
But the details show just how hard bigger reform will be. The amount established through an all-payer rate setting model ie as in Maryland or the qualifying payment amount. The Texas Department of Insurance TDI has adopted an emergency rule outlining the narrow circumstances when it will be legal for physicians to balance bill patients under the states new law that protects patients from.
In other words the qualifying payment amount is used for determining patient cost-sharing unless another state law or policy applies. This law protects patients from receiving surprise medical bills for emergency care or in certain circumstances unexpected out-of-network care. 1 2020 Washington state law protects you from surprise or balance billing if you receive emergency care at any medical facility or when youre treated at an in-network hospital or outpatient surgical facility by an out-of-network provider.
The bill also included languagethe No Surprises Actto address surprise medical billing. All congressional committees agreed on the end goal of protecting patients from. 3 2021 State Legislatures Magazine.
Bipartisan leaders reach a compromise. Consumer advocates have praised the law as one of the most robust set of billing. Once the legislation is signed into law doctors will no longer be able to charge emergency room patients unexpected exorbitant fees that must be paid out of pocket.
February 25 2021 ODI Governor DeWine signed House Bill 388 into law on January 7 2021. The new law isnt intended to preempt state surprise-billing laws but there is ambiguity in the statutory language that will require further clarificationincluding as to when these protections apply to patients in self-funded plans regulated by the federal Employee Retirement Income Security Act of 1972 ERISA according to the AMA guide. The qualifying amount will likely apply in many if not all.
Patients get surprise medical bills when they get care from a doctor lab or other provider outside their health plans network. The New Surprise Billing Law Is an Imperfect Win. Someone has surgery or gets treatment at an in-network hospital or facility but gets care from an ER doctor anesthesiologist radiologist or other provider who doesnt have a contract with their health plan.
In-network cost sharing for surprise bills will be based on a recognized. State Adopts Emergency Rule on Surprise Billing Law. The coronavirus aid bill contained legislation to end surprise medical billing almost exactly one year after the first major push to fix the issue collapsed at the last minute.
The law requires surprise bills must be covered without prior authorization and in-network cost sharing must apply. On December 22 Congress passed the surprise billing legislation as part of HR. By Haley Nicholson Feb.
This update reflects changes made to the surprise billing provisions after the agreement was announced on December 11. A new Texas law that aims to protect patients from receiving surprise medical bills takes effect this week. On December 11 2020 leaders of the Senate.
What the surprise billing law means for US. Health care The spending bill passed by Congress on Monday included a legislation that will help put an end to surprise medical bills. Surprise medical billing law.
133 the Omnibus Appropriations and Emergency Coronavirus Relief Act the large legislative package that closed out the 116th Congress. This most often happens in two situations. The new surprise billing protections apply to all commercially insured patients since public insurance programs like Medicare including Medicare Advantage and Medicaid already include.